Novel cancer treatment using drug release controlled by NIR-stimulated nanoparticles
27 September 2012
Controlled drug release at the site of a tumour using near-infrared stimulation of nanoparticles shows promise as a non-invasive treatment for deep cancer.
The research, by the Department of Bioengineering at the National University of Singapore (NUS) has been published online in Nature Medicine. This is a world first for the use of nanoparticles for non-invasive photodynamic therapy of deep cancer.
How does their technology work?
The team has discovered a way to control gene expression by using nanoparticles that are able to convert near-infrared (NIR) light to visible or UV light, which in turn causes a drug to be released. These nanoparticles can be introduced into target sites of the patient, where they can be activated.
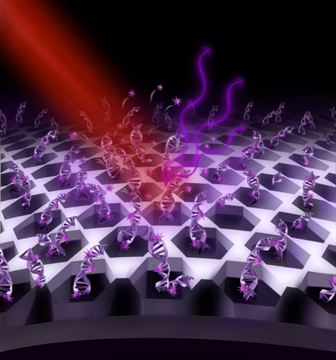
Schematic showing the process of NIR activating
drug release.
Genes release certain proteins in our body to ensure that our internal “machinery” works well and we remain healthy. However, sometimes, the process can go awry and cause our body to malfunction, leading to various disease. But doctors can put this right by manipulating the process of gene expression by using UV light. However, UV light may cause more harm than good.
Assoc Prof Zhang, the team leader, said: “NIR, besides being non-toxic, is also able to penetrate deeper into our tissues. When NIR reaches the desired places in the body of the patient, the nanoparticles which we have invented, are able to convert the NIR back to UV light (up-conversion) to effectively activate the genes in the way desired — by controlling the amount of proteins expressed each time, when this should take place, as well as how long it should take place.”
Their findings from this study were earlier published in Proceedings of the National Academy of Sciences, USA in May 2012.
As the up-conversion nanoparticles can also be used to produce visible light, the team has extended its application to other light-based therapies. Conventional light therapy for treating tumours uses visible light to activate light sensitive drugs that can kill cancer cells. However, such visible light is not penetrative enough to reach deep-seated tumours. The team’s method of employing NIR is able to penetrate much deeper. The team’s findings have been published online in Nature Medicine.
Their novel use of nanoparticles made news in 2010. Coated with mesoporous silica, these particles are each tasked to conduct “up-conversion”. Their paper “Multicolour Core Shell-Structured Up-conversion Fluorescent Nanoparticles” was published in Advanced Materials in December 2008. It was one of the most highly-cited papers because of its relevance in today’s science.
Wide range of applications
“By using our nanoparticles, drugs can be activated by NIR light which is safe. The light is also able to penetrate deeper into tissues to treat diseased cells," said Assoc Prof Zhang.
Co-author of the paper, PhD student Mr Muthu Kumara Gnananasammandhan added that what they have developed is a platform technology which can be customised for a wide range of applications. For example, in addition to photodynamic therapy, their innovation can also be used for bioimaging where the nanoparticles can be attached to biomarkers, which will then attach to cancer cells, allowing for better imaging of tumours and cancerous cells.
The six-member team comprises researchers from the faculties of Engineering and Science, as well as the NUS Yong Loo Lin School of Medicine.
The team is currently in collaboration with researchers at the National Cancer Centre Singapore to pursue a project funded by the Agency for Science, Technology and Research (A*STAR) that will assess the safety and efficacy of the technology to pave the way for pilot clinical trials in the future.
The team has also embarked on several other projects that make use of the up-conversion nanoparticle for point-of-care diagnostics for diseases. They have received the proof-of-concept (POC) grants from the Biomedical Engineering Programme (BEP) which is funded by the Science and Engineering Research Council (SERC) at A*STAR and the National Research Foundation, to develop these point-of-care diagnostic kits for rapid detection of bacteria and biomarkers.