Genetic analysis of Candida glabrata shows new genetic sources of drug tolerance
20 August 2014
The Max F. Perutz Laboratories in Vienna has coordinated a genetic study of Candida glabrata that has discovered 28 new genes that are partly responsible for the yeast's tolerance of common drugs.
The working group led by Karl Kuchler at the Max F. Perutz Laboratories (MFPL) — a research and training centre run jointly between the University of Vienna and the Medical University of Vienna at the Vienna Biocenter Campus — coordinated the international study aimed at researching new tolerance and virulence genes in Candida labrata. During this process, genetic methods were used to generate one of the world's three largest libraries of "knock-out fungi". More than 600 fungus mutations were created from which a single gene was specifically removed.
Now published in the journal PLoS Pathogens, the molecular analysis of the Candida glabrata fungus mutations revealed 28 new genes that confer anti-fungal tolerance, especially to the popular drug Caspofungin. The study, in which the coordinators in Vienna also collaborated with groups from the Johns Hopkins University, the Institut Pasteur in Paris, the Fraunhofer Institute in Stuttgart, Imperial College in London and the Genomics Institute in Barcelona, also identified new intra-cellular stress sensors and signal transmitters in Candida glabrata. Removing these characteristics genetically leads to marked sensitivity to all of the anti-fungal medications currently used in clinical practice — including Caspofungin.
"Since genetically removing these virulence factors from a Candida glabrata patient isolates markedly reduces their virulence as well as dramatically increases the fungal pathogens' sensitivity to medications, these signal transmitters are the best points of attack for the development of new and highly effective anti-fungal therapies," says Karl Kuchler from the MFPL.
"These findings represent a new milestone in the discovery and characterisation of Candida glabrata resistance genes, laying the foundations for the development of new anti-fungal medications. This means that, in future, it will be possible to treat the often fatal invasive infections with pathogenic fungi in a more targeted and efficient manner."
A few dozen types of harmful fungi claim more than 1.5 million human lives every year. Especially people with a severely weakened immune system are at particular risk of infections with yeasts of the Candida species, with invasive infections being fatal in around 40% of cases. Medications are expensive, and fungi are increasingly developing resistance.
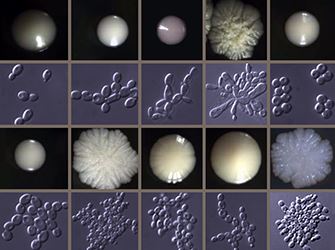
Fungal cultures
Worldwide, more than €8 billion is spent worldwide on anti-fungal medications, and the overall costs of treating the conditions caused by pathogenic fungi exceed hundreds of billions worldwide. The second-most common Candida fungus harmful to humans, Candida glabrata,, is a major clinical problem since it has sophisticated natural tolerance and can demonstrate resistance triggered by anti-fungal therapy to the most important medications.
As a result, infections with Candida glabrata need to be treated with very expensive drugs such as Caspofungin. Caspofungin blocks the biogenesis of components of the carbohydrate-rich cell wall, which is only found in fungi. The treatment of Candida glabrata, however, is becoming increasingly difficult due to the fact that anti-fungal resistance is common, the costs of Caspofungin are very high and because the frequency of infections with Candida glabrata has increased tremendously.
Reference
Schwarzmüller T et al. Systematic Phenotyping of a Large-Scale Candida glabrata Deletion Collection Reveals Novel Antifungal Tolerance Genes. PLoS Pathogens 10: e1004211. doi:10.1371/journal.ppat.1004211